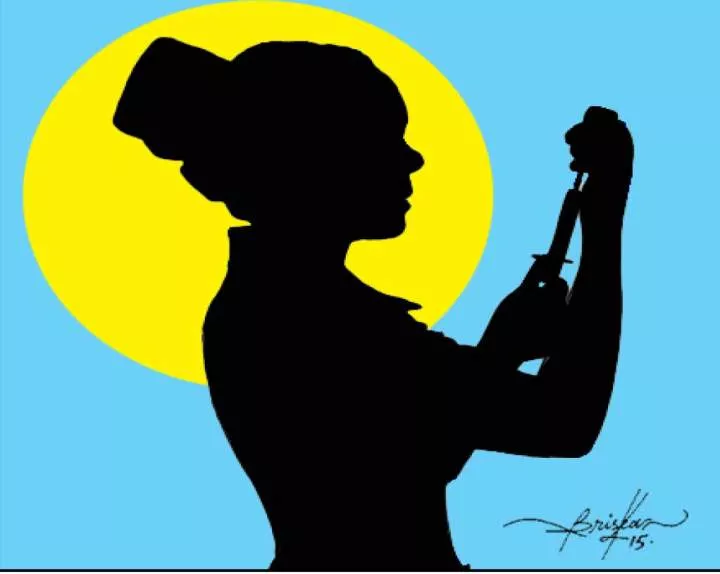
How does the new R21/Matrix-M vaccine work and where is it being administered?

The Ivory Coast has received the first doses of malaria vaccine from the world's largest vaccine maker, the Serum Institute of India, in collaboration with the University of Oxford, and began rolling out a new vaccination drive across the country earlier this week.
Malaria remains a significant health issue in the Ivory Coast, causing up to four deaths per day in the country with a population of 28 million. According to a 2022 report from the World Health Organization (WHO), malaria causes more than 600,000 deaths worldwide per year with 95 percent of cases occurring in Africa and 80 percent of those cases in children under the age of five.
Keep reading
list of 4 items list 1 of 4 list 2 of 4 list 3 of 4 list 4 of 4 end of list
A total of 656,600 doses of the new R21/Matrix-M malaria vaccine have been delivered to the Ivory Coast, where clinicians will initially vaccinate 250,000 children aged from newborn to 23 months across 16 regions, the government said.
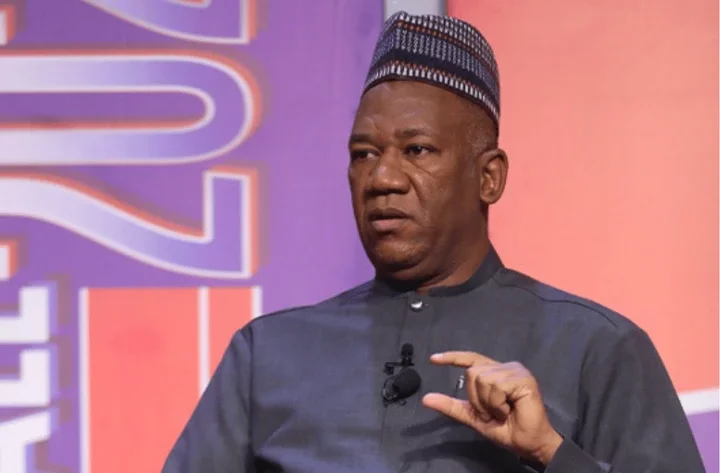
Professor Adrian Hill, Lakshmi Mittal professor of vaccinology and director of the Jenner Institute at Oxford University in the United Kingdom, told the media on Monday that the drive had been made possible through a joint initiative with the Serum Institute of India because of its "scale" and ability to mass-produce millions of vaccines at low cost.
After vaccines are rolled out in the Ivory Coast, the drive will move to other African countries, starting with Burkina Faso, Professor Hill said.
According to Gavi, an international health organisation which works alongside WHO and UNICEF, 15 African countries are expected to roll out malaria vaccines in 2024. Countries plan to reach about 6.6 million children with the malaria vaccine in 2024 and 2025.
Here is what we know about the malaria vaccine drive so far:

Which malaria vaccine is being used?
Health workers are administering doses of the R21/Matrix-M malaria vaccine, the second malaria vaccine to have been approved by the WHO in December last year, in Ivory Coast vaccination centres.
Research suggests R21/Matrix-M can reduce symptomatic malaria cases by 75 percent in a community in the 12 months following a three-dose series, with efficacy sustained by a fourth dose administered a year later.
"Over 600,000 deaths mainly amongst children are caused by malaria each year. The disease presents a uniquely difficult scientific challenge: the complex composition of malaria parasites with shape-shifting pathogen that has learned how to evade our immune system, has made the development of an effective vaccine a formidable task," Professor Hill said in a statement last December.
"R21/Matrix-M represents the culmination of 30 years of collaborative research and development by the University of Oxford Jenner Institute and, since 2017, in partnership with the Serum Institute of India."
The WHO and local health authorities are also delivering shots of the Mosquirix vaccine, also known as the RTS,S malaria vaccine, to more than 2.3 million children across Africa this year.
This vaccine has been primarily introduced in Cameroon, Ghana, Kenya and Malawi, focusing on children aged five months and older in regions with a significant prevalence of Plasmodium falciparum malaria.
How does the R21 vaccine work?
The R21 vaccine uses adjuvant technology, which enhances the immune response to the vaccine, allowing protection from future infections of a disease.
The vaccine is designed to specifically target the sporozoite stage of the malaria parasite. This is the initial form of the parasite that enters the human body when bitten by a mosquito. By focusing on this stage it helps to boost the immune system's response, leading to higher efficacy in preventing malaria. In addition, the vaccine can prevent the parasite from infecting the liver and causing illness.
How widely available is the vaccine?
The Serum Institute of India, which was responsible for delivering more than 2 billion doses of COVID-19 vaccines around the world, is capable of producing 100 to 200 million doses annually, making it more cost-effective and accessible. Professor Hill told the UK's BBC Radio Four Today programme on Monday that the Serum Institute's ability to mass-produce vaccines had reduced the cost of each R21/Matrix-M shot from about $8 or $9 to about $4.
It will also be made available in several other African countries. "The new vaccine has been authorised by Ghana, Nigeria, Burkina Faso and the Central African Republic, and many others are preparing to receive shipments," the University of Oxford said in a statement to CNN.
How can malaria be eliminated?
The goal set by the WHO Global Malaria Programme (GMP) is to reduce cases of malaria by 90 percent by 2030.
Measures in place to achieve this are:
Early detection and diagnosis of malaria cases to prevent transmission and deaths.
The effective mass distribution of affordable vaccines in countries with high infection rates.
The use of insecticide-treated nets (ITNs) and indoor residual spraying (IRS) to reduce mosquito populations and transmission through mosquito bites.
Building awareness about the disease and how it spreads and how to treat it in malaria-prone communities while ensuring proper access to the necessary health facilities.
According to the WHO report, however, some challenges remain. "Countries, subnational areas and communities are situated at different points along the path towards malaria elimination, and their rate of progress will differ depending on the level of investment, biological determinants (related to the affected populations, the parasites and the vectors), environmental factors, strength of health systems, and social, demographic, political and economic realities," the report states.













Comments